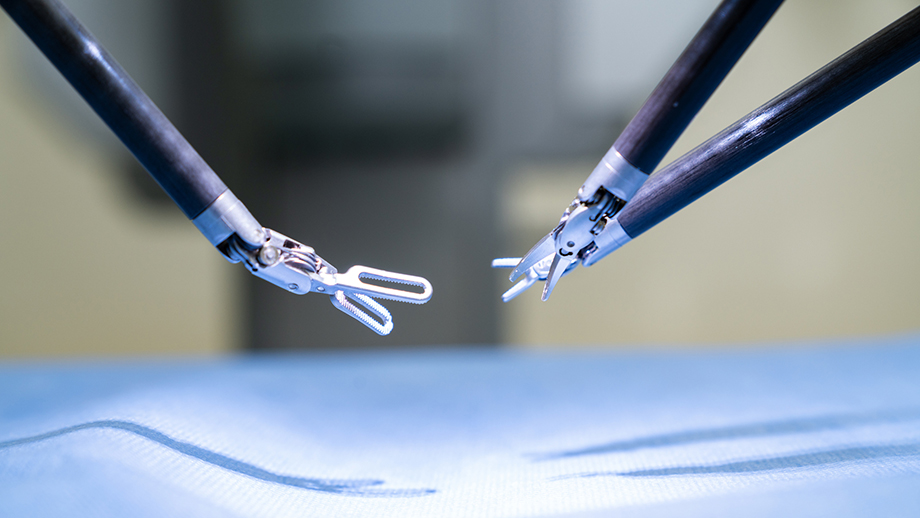
Surgical Director of Adult Liver Transplantation and Chief of Hepatobiliary Surgery, Jason Hawksworth, MD, is one of the few surgeons in the United States doing complex liver surgery entirely with the robot. It’s an incredible evolution in how surgeons can approach the organ itself. Procedures that could never be done on a liver with other minimally invasive techniques can now be done robotically.
An expert who built the Robotic Surgery Program at Georgetown University Hospital, Dr. Hawksworth joined Columbia’s Center for Liver Disease and Transplantation this summer.
We’re thrilled to welcome his passion, dedication, and leadership to our patients in New York City, the Tri-State area, and beyond. In this interview, Dr. Hawksworth shares how his love for robotics began and the many benefits robotic surgery provides for patients—from shorter hospital stays to pain management.
What brought you to robotics? Were you always interested, or did that focus evolve?
It's interesting. I've been practicing abdominal transplants and hepatobiliary surgery since 2010. Initially, my practice was mostly traditional open liver surgery and transplant surgery. That's how I was trained, and most people are still trained that way, to be honest. I had a little bit of exposure to laparoscopy, both in general surgery residency and also in fellowship, but very limited, mostly laparoscopic kidney surgery. Some surgeons were doing a hybrid laparoscopic approach to liver surgery, hand-assisted. You'd still make an incision so you could put your hand in and then use the laparoscopic instruments just to try to keep the incisions a little bit smaller.
Safety is a big thing with liver surgery because it's dangerous, and there's a mortality risk in the operating room, so you must be careful about trying new things. My practice evolved from mostly open to hybrid hand-assist. And then, over time, I felt more comfortable doing more things totally laparoscopic. But I was limited to smaller cases like minor hepatectomy [removing part of the liver], and I couldn't really do anything complex.
Do you mean you can’t access certain parts of the body laparoscopically or make certain movements?
Laparoscopy is very limited. The camera is two-dimensional, so you have no depth perception. The instruments don't articulate, meaning you can't move the instruments in a way that your hand would normally move. They're straight instruments.
You operate in a closed space, and your optics are very limited. Your instrumentation is very limited. You're working with straight sticks, so it's very hard to dissect around vessels, for example. It's hard to get behind the liver. The limitations turn into safety issues because, in liver surgery, you have to be able to deal with bleeding problems, which are common. If you don't have the expertise laparoscopically to fix a bleeding complication, you and your patient can get into a lot of trouble.
I felt limited in what I could offer patients safely. So, I trained on the robot in 2018. It took me about six months to learn the platform and be comfortable with it. I would practice on the robot when I had time at 2 a.m., and did case observations with some other surgeons that were already doing robotic liver surgery. There were only a handful of people doing it in the whole country, and still, only about a dozen of us actually do complex liver surgery robotically. It took me a long time to get comfortable and be able to really do it well.
Once you feel comfortable on the robot, how do you start transitioning to robotic surgery in the OR with patients?
Once you learn the platform, the system, the technology, you can very quickly increase the complexity of the types of cases you're doing, and that's what I found with the liver. I went from doing minor hepatectomies laparoscopically to basically being able to do 90 percent of my liver work robotically. I still do some open hepatectomies, primarily for very large tumors where you have to make a big incision and take it out anyway, so it doesn't make sense to do it robotically. Or if there's a vascular problem from the tumor—that's still very hard to do minimally invasively. Outside of those two scenarios, I'm doing everything robotically.
When it comes to liver surgery, what are the benefits of the robotic approach?
The difference in outcome is drastic. I have a lot of this data that I've presented at meetings, and I'm going to have it published soon, but the length of stay after an open hepatectomy is between five and seven days, whereas the length of stay after robotic hepatectomy in the exact same case is between two and three days.
Wow.
It's literally cut in half. Patients don't require a lot of narcotics. They almost never require IV narcotics in the hospital. The blood loss is statistically significantly less. Complications, particularly major complications, and major morbidity, are statistically less, and the oncologic outcomes are the same.
You're still getting curative liver surgery in the vast majority of cases, and it's no different than open. You're not losing anything. It really changed my practice.
You’re the first robotic liver surgeon at Columbia; what are your goals for the program looking forward?
There are two areas that we're focusing on right now. One is building the liver cancer program, Columbia’s first multidisciplinary liver tumor clinic. We'll have hepatobiliary surgery, medical oncology, and interventional radiology. All of the providers that patients need to see for their specific problem will be in one place. They don't have to make four or five different appointments, come up with a plan, and then execute it.
And hopefully, that will translate into more patients in clinical trials. More patients getting robotic liver surgery, if that's appropriate. More patients getting local regional therapy by interventional radiology. Or no observation in some cases and just good follow-up. And then, in some cases, transplant.
That’s great. Speaking of transplants, is that your other robotic focus?
Yes. The other component is adapting robotics into transplant. Specifically, we're going to start doing some of the living donor hepatectomies robotically. That will be great for donors who are healthy people and don't want a giant liver incision. It'll help them recover faster, get back to work, get back to their lives faster, and still provide the same safe operation with a viable liver segment that could be transplanted into their loved one or friend, or however that's being arranged.
Do you see the possibility of robotic surgery on the liver recipient in the future, too?
The recipients are all open at this point. I think in the future, we will be able to do some liver transplants robotically, but I don't think that that's going to be mainstream for a long time, in my opinion.
Is that because of the size of the liver?
The liver is giant. You end up either doing an incision on the upper abdomen or a big C-section type incision. There are definitely limitations to that, especially when you're talking about a whole liver. A liver segment is probably more doable, but that will take a lot of development.
Now, we’re doing robotic kidney transplants. Dr. Ratner started that here at Columbia. I was doing those in DC, and I've been doing those for about a year, too. But my interest is in the liver.
What makes the liver so intriguing to you?
The liver is more challenging than the other abdominal organs. It's truly lifesaving because there's no dialysis for liver failure. If you're sick from liver disease, transplant is your only option in most cases. And patients do really well after a successful liver transplant. It's like night and day when you look at a sick liver patient and then see them three months later after a successful liver transplant. They literally look like a new human being. It's pretty cool.
Speaking of challenges, you were in the military, worked at Walter Reed, and deployed to Afghanistan. Did that experience have a big effect on your passions and practice as well?
Every medical and surgical experience you get makes you a better practitioner. You learn something. I think on deployments, you're very resource-limited, so you have to innovate a lot to do things that normally would be easy in a modern hospital.
In Afghanistan, for example, you're in a tent, so you're trying to operate in a tent. It does make you innovate, understand resource limitations. Being able to triage increases your speed, particularly in a trauma situation. It probably made me a better surgeon.
Further reading:
- Caracas to Santo Domingo: Creating Access to Pediatric Liver Transplant from the Ground, Up
- The End of the Liver Wars: A Victory in the Battle for Liver Transplant Equity
- By Letting Patients Lead, We Can Advance Medicine
Sign up for our mailing list for more health news and information from Columbia.