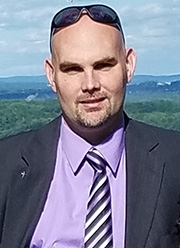
Joe benefits from next generation LVAD and heart transplant
 At 19, Joe de Rosa was working as a patrol officer and Emergency Medical Technician. One day, he had trouble breathing—even a little exercise suddenly left him winded. At about the same time, he also felt a lump in his neck. Joe was shortly diagnosed with acute lymphocytic leukemia, a life threatening cancer of the blood.
At 19, Joe de Rosa was working as a patrol officer and Emergency Medical Technician. One day, he had trouble breathing—even a little exercise suddenly left him winded. At about the same time, he also felt a lump in his neck. Joe was shortly diagnosed with acute lymphocytic leukemia, a life threatening cancer of the blood.
After three and a half years of chemotherapy, enduring hair loss and leg pain so severe he couldn’t walk without a cane or brace, Joe miraculously rebounded. When he learned he was in remission, he took a job as a grounds engineer in the town of Poughkeepsie, overseeing landscaping and building maintenance.
“For 15 years after my cancer, I worked hard and led a normal life,” Joe recalls. “Then in the summer of 2015, I had trouble breathing again. A pulmonologist didn’t find anything but by following February, I was exhausted and having trouble keeping up with the demands of my job.”
On his lunch hour, Joe went for an echocardiogram and learned that his heart was only beating at 25 percent of its capacity—a side effect from his chemotherapy years before. He was sent directly to Vassar Brothers Hospital. After more tests, Joe’s medical team knew there was nothing more that they could do so they transferred him to NYP/Columbia and the most experienced heart team in the world.
Dr. Melana Yuzefpolskaya evaluated him the day he was admitted. “Joe was in shock, very ill, and obviously in need of a heart transplant,” she recalls. “Unfortunately, an organ was not readily available and to buy him time, we proposed a Left Ventricular Assist Device (LVAD)—a mechanical pump that would be implanted in his chest and assist the function of his struggling heart.”
Columbia was then the principal site for the study of a new, more efficient LVAD, a pump called the Heartmate 3™. Joe agreed to participate in a clinical trial of this new device and Dr. Yoshifumi Naka implanted one in Joe’s chest in April 2016.
“I did very well on the Heartmate 3,” Joe says. “The first month or two, I felt almost normal. I was walking and was never out of breath.” The LVAD functioned as a bridge to transplant, and Joe got his new heart shortly after midnight, on October 3, 2017.
“For eight days I was on ECMO—a machine to support for my heart and lungs—then I went to a regular room to convalesce,” Joe says. “I went home after total of just 15 days.”
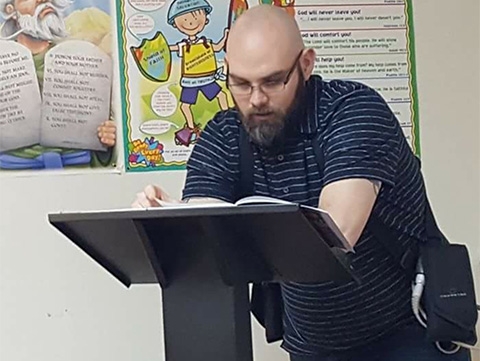
As he adjusts to his new heart, Joe serves as a youth minister at his local church. He also plans to go back to school. “I’m thinking of a career in information technology, or civil service,” he says. “Maybe even a desk job at the local police department.”
The Heartmate 3 study, led by researchers at Columbia was completed about the same time as Joe’s transplant. This life-saving device is now FDA approved for patients with advanced heart failure awaiting a transplant just like Joe did.
“Joe is a survivor,” says Dr. Yusefpolskaya. “At 36, he has overcome two potentially fatal illnesses with enviable dignity and grace.”
