By Cale Li, MD
When making decisions about heart surgery, you would want all the facts. Putting your trust, and heart, in someone else’s hands is not easy. You’d probably want to know how good the surgeon is–but what does that mean objectively?
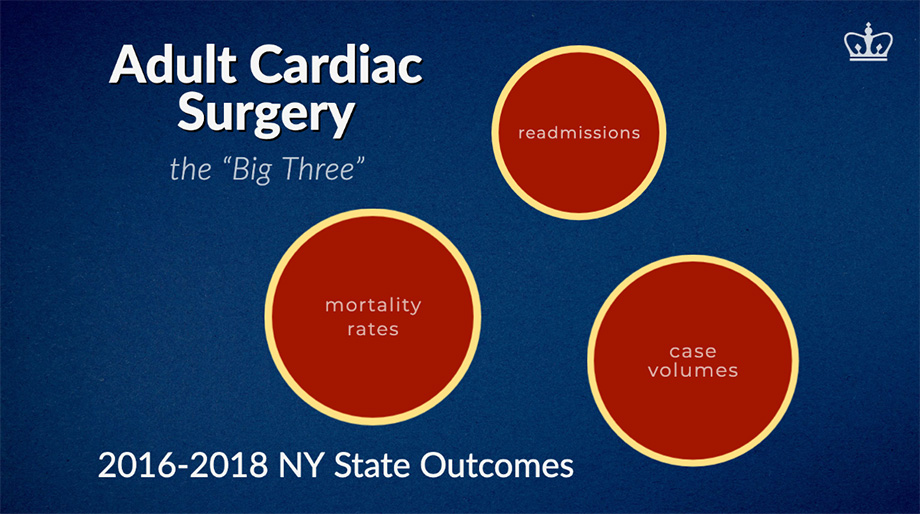
In the 2016–2018 cardiac surgery outcomes report, New York State (NYS) examined three major measures of quality:
- mortality rates – how many patients die from surgery
- readmission rates – how many patients get re-admitted to the hospital after surgery
- volume – how many heart procedures are performed by the hospital
“The [NYS cardiac outcomes] results reflect some of the things that are most important to patients: what is the chance I die? Will I need to come back to the hospital? How many procedures are being done at the center?,” said Isaac George, MD, Cardiac Surgeon and Surgical Director of the Heart Valve Center at Columbia.
Data is an invaluable tool for patients seeking to make an informed decision about their healthcare.
“You can use this data to help your loved ones get the best possible outcome: leave the hospital alive, leave the hospital in good condition and not have to come back, and be at a center with experience to handle complications, unexpected events, and complex situations.”
The likelihood of dying from surgery is defined as the mortality rate. For a complex cardiac surgery like coronary artery bypass graft (CABG), the overall 30-day mortality rate was 1.48%.
“Unquestionably when it comes to cardiac surgery, the most important measure of quality is mortality,” said Paul Kurlansky, MD, Associate Director of Research, Recruitment and Continuous Quality Improvement. “When undergoing potentially life-saving surgery, the most important question patients need answered is what are my chances of surviving the operation?”
The report goes on to list the observed mortality rates at each individual hospital. Over 416 surgery cases, New York Presbyterian – Columbia had an observed mortality rate of 0.72%.
Comparatively for institutions with similar case volumes, Buffalo General Medical Center had an observed mortality rate of 1.90% over 455 cases; Rochester General Hospital with 2.78% over 396 cases; Lenox Hill Hospital with 1.37% over 366 cases.
Similarly, paying attention to case volume can help determine the level of expertise of a surgeon.
“Volume helps patients to understand the level of experience at various institutions,” said Dr. Kurlansky. “There is a strong correlation of volume with quality…it is essential to know both parameters in order to more completely assess the expertise of any given surgeon or surgical center.”
A hospital that performs a high volume of heart operations, while maintaining a low mortality rate, indicates quality of care.
“In the area of coronary bypass surgery, the most commonly performed operation in the State, CUIMC had the highest volume of any of the centers in NYC with a mortality approximately one half of what would be expected for the complexity of the patients who had this operation. Similarly, mortality was one half of the state average,” said Dr. Kurlansky.
“For TAVR (transcatheter aortic valve replacement), for which Columbia was one of the world leaders in the development of the technique, Columbia has the highest volume with the lowest mortality of any hospital in NYC–and is the only one in the city with distinction of having a mortality that is beyond the statistical limits of differentiation, nearly one half of what would be expected.
For Dr. George, the key to success is the culture of collaboration. “Columbia is a special place for cardiac surgery. We have the collective excellence of a group of doctors, surgeons, anesthesiologists, imagers, PA/NP, nurses–dedicated teams to provide personal, world-class care to every patient. We constantly monitor our results and strive to make our centers better and better.”
“It’s not a coincidence that Columbia excels in volume and quality,” said Dr. Kurlansky. “As a major academic medical center, Columbia is a leading center for innovation in the development and perfection of emerging techniques and methods of patient care. Moreover, Columbia has a unique culture of collaboration between cardiology and cardiac surgery which provides the patients with the optimal treatment according to the highest standards of the profession.”
New York Presbyterian – Columbia ranked among the top institutions in mortality rate and case volume, but its readmission rates were above the state average for CABG. But while mortality rate and case volume are fairly straightforward metrics (fewer deaths and more experienced surgeons), readmission rates can be a more nuanced metric regarding quality of care.
“Readmission has been promoted as a metric of quality. I disagree–it is a metric of utilization, not necessarily quality,” said Dr. Kurlansky.
“It is true that if there are unresolved issues of care at the time of patient discharge, or if the patient has not been appropriately engaged regarding best care following discharge, the risk for the need for readmission increases. In that sense, better communication and planning can help to reduce the need for readmission, and does in fact represent a better level of care. That said, we care for sick people and sometimes the best care requires that people be readmitted when they develop disease-related problems.
“[For example] after the Centers for Medicare and Medicaid Services imposed institution penalties for readmission for congestive heart failure, readmissions went down but mortality actually went up. In other words there was an inverse relationship between readmission and mortality in the care of patients with congestive heart failure (a phenomenon which the Cleveland Clinic had previously published in a letter to the New England Journal of Medicine).
“So, in fact, readmission may, on the one hand represent a deficit in care–or, on the other hand, may represent the optimal care of a sick patient. Given all of these factors, I think that it is fair to say that, as a quaternary referral center, we tend to operate on a sicker and more complex group of patients for whom readmission may be the optimal way to fulfill their medical needs.”
The full cardiac surgery outcomes report is available for public access.