An interview with Yuri Novitsky, MD, Director of the Columbia Hernia Center, and Dina Podolsky, MD, hernia surgeon.
What’s new in surgical approaches to hernia repair?
Dr. Novitsky: Well, what's new is actually the entire field of abdominal wall surgery. We're witnessing the creation of and recognition of what we do, deservingly as a specialty. And now, people's careers are dedicated to this craft of abdominal wall surgery.
So before we even dig into what we do, just the fact that we run the Columbia Hernia Center with 95 percent-plus of our practice centered on hernias is what's probably very new in the world of surgery.
Dr. Podolsky: Yeah, for us, that question is twofold. It involves both the techniques that we use and the actual surgeries themselves. What we bring in terms of newness is the robotic approach to almost any type of surgical repair, and we do that consistently at Columbia.
And then there are the actual techniques. We are cutting-edge in a new field that's being developed. We are part of academia; we are a part of the current change.
Let’s talk robotic surgery. How has that advanced hernia repair? What are the benefits of the robotic approach for patients?
Dr. Podolsky: Robotic surgery allows us to do the most complex surgeries with a truly minimally invasive approach. Laparoscopic surgery allowed us to do a lot via a minimally invasive approach, but it was limited in terms of the complex abdominal wall reconstruction—the sewing on the ceiling of the abdominal wall, doing these really big hernia repairs with just a couple of small cuts. So robotic surgery allows us to say, "Nothing is off the table" when it comes to minimally invasive surgery.
Dr. Novitsky: The trends of minimally invasive surgery—meaning small incisions, faster recovery time, less scarring, fewer infections, so the group of techniques that we call minimal invasive surgery—involves both laparoscopy and robotic surgery. We’re expanding laparoscopy like Dina just said. So, now we're actually approaching almost every patient with robotics in mind as our first procedure method. Starting there, then determining the best choice for them.
It's changed our own personal algorithms in procedure and technique selection. So not only has robotics allowed us to apply minimal invasive surgery to a broader range of patients, we also feel robotics has significantly improved pre-existing laparoscopic techniques. It allows us to place the mesh outside the peritoneal cavity and allows precise closure and reconstruction of abdominal wall defects, which was very difficult, if not impossible, using the traditional laparoscopy of the early 2000s.
But what's different about us is that we rarely utilize straightforward, old-fashioned laparoscopy approaches to both routine and complex defects and use cutting-edge techniques to address a broad range of hernias, from first-time to multiple recurrent, and everything in between.
Wow, interesting. So, this isn’t just about surgical procedure preference. Robotics is changing what hernias you can repair and how.
Dr. Podolsky: Absolutely. The algorithm has changed. Even when I was a fellow a couple of years ago, I was still approaching complex stuff with an open-first mentality, and which ones can I squeeze in robotically. Now it's almost, "What's the reason that I can't do this robotically?" I need an actual reason.
Dr. Novitsky: It’s a key point of transformation. And as surgeons, we both have almost a full spectrum of procedures in our armamentarium. We can select the most appropriate procedure and certainly have algorithms to determine how we go about it. We don't just try to fit everybody into the same one operation, one approach. Patients have different hernias. The goals of both our patients and us vary.
It sounds like robotics is actually transforming aspects of hernia surgical repair. How is the way you use robotics different from how other specialties may use robotic surgery?
Dr. Novitsky: Well, to offer the robotic procedure, it requires certain things: the knowledge of how to do it, the desire to learn to do it, the skill that is necessary to obtain to do it. And depending on your career point, it gets harder and harder to go back to school and learn a whole new technique, new technology. Have a learning curve, be a little bit slower at the beginning and then gain that experience that equals your traditional kind of approach. I had to do that because I had to adopt robotics mid-way through my career.
Dina was in her training, so she was learning robotic techniques. Her approach is very different because she learned that way, and she's so comfortable doing and offering it. You may hear often people putting it down or doubting it, mostly because they're biased by lack of ability to do it. And we hear this all the time, whether it's laparoscopy or robotic surgery, "Oh, I don't need it, I can do that through a small cut."
The truth about robotic surgery is that the knowledge and experience are evolving. It’s a very new procedure, so they have a point when they want to criticize or point out the lack of clear-cut randomized data. We're learning. But it’s a no-brainer for us who do it every day and see the benefits for our patients, the precision of our work, and the outstanding results that we produce. And that's why it leads to us doing more and more.
In fact, sometimes it's more challenging, it's harder to do, it takes a little bit longer, but we put in that effort because the view is worth the climb. At the end of the day, when you're done with a procedure, the patient is better off, and we as surgeons feel more satisfied that we’re doing the best job possible for a given patient.
Tell us about your selection process, the algorithm you use to decide when and how to select robotic surgery over other approaches.
Dr. Novitsky: Well, ventral hernia patients are approached differently than groin hernia patients, so we’ll start with ventral hernias, the abdominal wall.
Dr. Podolsky: First, you always just look at the person overall. How healthy are they? What medical problems do they have? What's their surgical history? The basics. And then, you discuss what your patient’s goals are and what their needs are. You look at their problem, the hernia that they have, and you do that through a combination of a physical exam and imaging studies. I put that all together, and I see what's the best solution to this possible problem.
Like I mentioned earlier, there has to be a good reason that we don't do it robotically because we see the clear-cut benefits—waking up with just a couple of cuts, staying in a hospital one or two days instead of a week, really reducing the risk of infection and all these other things that can happen to surgical patients.
Dr. Novitsky: All while providing a very precise repair on the inside. You're accomplishing challenging steps using a minimally invasive technique. People who do laparoscopy say, "Well I do it through small cuts," but they can't do what we do robotically through small cuts.
Dr. Podolsky: I just had a patient who carries a lot of weight, is a bigger person, and she was not able to lose the weight, but she had a problem with this hernia. So sometimes, as a physician, I just have to do the surgery. You’ve got to do the right thing for the patient. And I was explaining to her that because of her size, it would be easier for me and her post-operatively to get it done robotically instead of open. And at first, she had a hard time in her mind because she thought I was going to do a different operation. But it was really fun to explain to her that we could do everything the same way—every bite is the same, every stitch is the same, you just wake up without a giant cut in your belly.
Dr. Novitsky: That’s it. We tailor our techniques to patients, so it's not a cookie-cutter practice where we offer the same operation to patients again and again. Not everybody proceeds to surgery right away; some people require careful pre-operative preparation with imaging, counseling, weight loss, diabetes management, smoking cessation. We take those steps to optimize and make them better because we want them to be in the best shape possible for this operation. Some people can't wait for that to happen, so they would accept slightly higher chances of certain complications, but those are still reduced if minimally invasive surgery is utilized.
What is the cookie-cutter approach? How do your tools, even beyond robotic surgery, differ from what most surgeons are doing elsewhere?
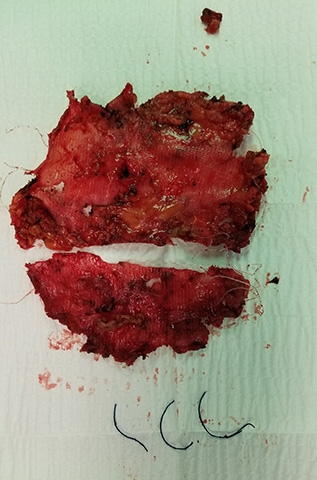
Dr. Novitsky: For a hernia surgeon, for an abdominal surgeon, to have a successful operation, I always break it down into three main ingredients: the patient, mesh material, and surgical technique. We already mentioned our ability to recognize and guide people through the pre-operative optimization process to ensure they're in the best shape possible for that operation. We also have a very precise knowledge of modern biomaterials. I have years of research and publications about different material types, so we're able to figure out which type is better and utilize what I feel are the best materials, especially for particular situations. We shy away from some popular, expensive meshes that experience has shown don't work as well.
It’s about knowing which material is best for which patient, for which procedure. Even in our hospital, people use stuff they shouldn't be using all the time just because they don't know better. It’s something that they've learned when they were residents 20 years ago. But things have changed, And then surgical techniques vary from small operations when we just put a few stitches to larger operations when we put meshes into patients. And the trick to what we strongly believe is the location for that mesh.
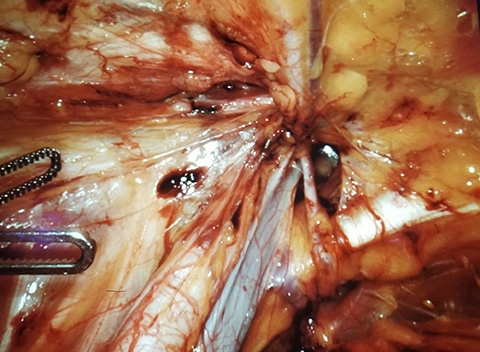
The most important asset is our ability to place prosthetic material in between the layers of patients' abdominal wall. So essentially we're able to separate certain layers of the abdominal wall to then put a prosthetic that is hidden away from the intestines, and yet far away from the surface, from the skin to prevent infections.
Our ability to reliably achieve those spaces between the abdominal wall muscles is what's really key here. We don't just go in there and patch a tire with a piece of plastic mesh; we actually create a pocket, suture the defect shut, put the prosthetic to reinforce as a patch, and then hide it from the rest of the body. It leads to fewer long-term complications and foreign body sensation infections, and also it doesn't interfere with subsequent operations.
So you’re doing an entirely different technique to repair these hernias?
Dr. Novitsky: It’s becoming one of the more common procedures worldwide, and what's important is that we do it right. We don't just say, "We do that procedure because we name it by name." We also know all the details. Dina and I see a large number of patients who've had these types of procedures done elsewhere, but they're not done correctly. An incorrectly performed procedure where the surgeon tries to separate the abdominal wall but doesn't do it correctly often leads to catastrophic complications and worsens the initial situation. By the time they come to us, they're a lot worse than they were before that failed operation.
How frequently are you doing re-operations?
Dr. Novitsky: At least half my practice is based on multiple recurring ventral hernias.
Dr. Podolsky: Yeah, at least 30 percent.
Dr. Novitsky: Hernia became a specialty for this reason. When I was in my surgical training, it wasn’t. Everybody thought they could do it, and they did. Even today at Columbia, colorectal surgeons, liver surgeons, transplant surgeons try to do hernia surgeries. Based on the mentality that it's not critical, “it’s just a hernia.” It's a complex problem that requires in depth understanding of the pathology itself as well as an in depth understanding of surgical options and execution of those complex techniques. So it's a multi-level problem, and our practices become more complex because the complications override those options. Often they're quite devastating for the patients.
And that's where we're at today. We’re fighting the prejudice that it's just an easy thing, and everybody should be able to do it. They watch a YouTube video of some complex technique without proper training and often create, as I said, catastrophic change and complications in the abdominal wall, not just failed hernia repair but really much more impactful missteps.
Dr. Podolsky: Yeah, I have to say, as a patient, you don't want to be coming to us with your third, fourth repair. It would have been better if we caught you the first time around, so you never got to hernia repair number three or four. Right now, we're still a bit in the salvage phase of things. A simple umbilical hernia can become an abdominal wall surgery if you don’t do it right.
And it's not the patients' fault. In much of this country, they don't have access to a place like the Columbia Hernia Center. It's really such a privilege to be able to provide this type of care, and it's something that should be utilized as much as possible.
Dr. Novitsky: Dina's right. And there are lots of people out there who do a good job. But a large proportion of people who can't. Many hernias are very common, and the specialists are still few and far between, and we’re working to change that. I'm on the executive council of America’s Hernia Society, and I lead the Practice Advisory Committee where we’ve created a lot of initiatives to try to educate surgeons and improve the overall hernia care nationally, internationally.
It sounds like your sort of fighting on two fronts of bias, physicians who say “it’s just a hernia” and the general public, patients who think the same.
Dr. Novitsky: You know, and a lot of times, they’re going to be right. There are some structural failures we see for routine stuff, but generally, routine, simple hernias go okay around the country.
But here’s the thing, even at Columbia, it’s not expertise-based credentialing for hernias. You don’t need to prove knowledge. Colorectal surgeons may clear hernias because they deal with a lot of complex patients, but by no means does it make them experts to fix them. But all colorectal surgeons continue to try, and it just shows you it's an uphill battle even when we're in the same building. So, imagine the uphill battle when we’re not in the same building.
Regarding abdominal walls, how does the surgical approach differ for the genders? Does hernia repair in women require a different approach at times?
Dr. Podolsky: Absolutely. Yuri and I have written a couple of textbook chapters on this very topic. Basically, it's a different approach because of the specific patient population of women of childbearing age. You have to really consider what would happen to their abdominal wall and what would happen to their body if they get pregnant and if you've done a hernia repair on them. We uniquely work in parts of the body that can change as people change, specifically with pregnancy, and that's something that most people haven't thought of.
There is dedicated work on this topic coming out, primarily out of Europe, showing that these patients need to be considered differently. For instance, you'd never want to put a big piece of mesh in a young woman's abdominal wall to fix a hernia because as they get pregnant, it can cause them pain and the pregnancy itself stretches the hernia repair so they’re at a higher risk for the hernia coming back after their pregnancy. You start thinking, “We should really save the heavy-duty or the more complex or the mesh-based repairs for when they're done having babies.” And that type of thinking is really new and probably not done by 99.5 percent of doctors out there.
Talk to us about mesh. What mesh do you use to repair hernias in women of this age?
Dr. Novitsky: Even when they do need mesh, some meshes can go away that don't last a long time, but they provide some repair stability. If you have a young woman of childbearing age, we really emphasize the need for proper non-mesh repairs to avoid any potential complications associated with mesh. Oftentimes, we have young fit women who come, and they're maybe seeking a second, third opinion. Some of the previous opinions involve laparoscopic ventral hernia repairs, meaning they're going to put a patch. And in 2008-2009 that was the standard of care. I've done that, and now, obviously, I have learned that it's just a bad idea.
We put a lot of mesh into people; we take out a lot of mesh from people for different reasons. So, we're very cautious about putting it in people unless we feel it's absolutely necessary. And I think that's probably the difference between many other centers and us. We're very selective in our use of mesh, the types of mesh we use, and the location where we place our meshes. There's something called lightweight, reduced weight meshes that are more pliable, that are a little bit less irritating to the body and the body tissues, so we do that a lot.
When you’re not using mesh, is it a suture repair?
Dr. Podolsky: Yeah, it would be a suture repair. For instance, your basic umbilical hernia, which is a hernia at your belly button, the majority of general surgeons in this country would likely use the mesh to repair it, even small ones. We don't because the data supports that the majority of people, even without a mesh for these small, primary belly button hernias would be fine, and we just use a suture. Sometimes one maybe two sutures. The procedure takes 30 minutes, no anesthesia. They’re in and out. The recovery is days maybe, and no narcotics are needed.
Dr. Novitsky: We know how to place the suture. We use very precise dissection techniques around identifying the hernia defect, identification of the tissues, and trimming, recognizing what tissue is healthy enough to hold the suture. It's not just make a quick cut, put a stitch and get out. We break down even those sort of trivial procedures in necessary steps and accomplish each step sequentially with proper dissection, proper tissue. I call it trimming, but it’s identifying healthy tissue that is good for suturing. And ultimately, as Dina pointed out, we don't put people to sleep, so they have a nicer wake-up without stressing our repair. They have a fairly uneventful recovery, it’s a very streamlined process.
Why do so many surgeons use mesh for things that don’t need it? Is it easier?
Dr. Podolsky: No, the short answer is that it's for multiple reasons. One, in traditional practice patterns, mesh has been used for a very long time, and the data still supports mesh in lots of different scenarios. For instance, incisional hernias, hernias that you develop because you've had a previous surgery, those almost always have to be fixed with mesh. So, there's still tons of indication with mesh, but at this point in the game, mesh is the safe choice, and you really have to have a ton of experience and security in what you do to move away from that, even in certain situations.
Dr. Novitsky: It's comprehension, and it's an understanding of options. We really consider a patient. We don't just have hammer and nail tactics here. We put a lot of meshes in people; we believe in the benefits of a mesh. By no means do we think mesh should be avoided at all cost, but it should be used sparingly and when it's necessary because we see the complications, and we know when it's not necessary.
It’s practice patterns. It’s dogma. It's how they were trained. Most people don't stay up to date on what's latest and greatest. And even the data could be misinterpreted. The data suggest that repairs with mesh are more effective, but when we take extra time and look at the numbers, we recognize that they're saying that the failure rate without mesh is 12 percent and the failure rate with mesh is 4 percent, and conclude "Hey, it's three times higher so everybody should be using mesh."
And to me, it's a huge number considering all the other potential complications. I'd rather have a small proportion of patients who have a recurring hernia, and we apply a larger repair the second time, or we would spare a large repair with mesh. That's part of our philosophy. We would like to avoid the biggest possible operation the first time when we can because we think these smaller repairs will not cause complications. They're not going to cause issues, pain, and infection, but they might, in a small proportion of patients, result in another operation.
Will you break down the different types of mesh and how you use them?
Dr. Podolsky: There are three categories that you could probably think of— Biologics are the mesh made out of either human dermis or parts of intestines, and those are the mesh that are completely broken down in the body. There's the synthetic mesh that is non-absorbable and stays in the body forever. Common materials are probably propylene which you can think of as a smooth plastic or polyester. And bioabsorbable meshes are the mesh that will act as a synthetic mesh for the first six, 12, 18 months, but then slowly be broken down via different ways in the body. Some people like to say it's the best of both worlds.
Historically, the first synthetic meshes were described in the 1950s, so we've got almost a hundred years of work with this stuff now. Biologics are nice meshes. They go away completely, they're very expensive, and you really limit their use to super emergency. They are not good in long-term repair. Synthetic meshes are our go-to for our elective, controlled big hernia operations where we want to make sure we fix this hernia once and never again, and the bioabsorbable is the one in between.
We're finding new places to use them all the time—for instance, those young women who need hernia repairs. You want to make sure you give them a good repair at the beginning, but maybe not leave a mesh in their body forever. That would be the new way to think about using the bioabsorbable.
Dr. Novitsky: And there’s been a bit of a renaissance with the use of synthetic mesh. The biologic meshes came out for the abdominal wall in mid-2000 and became very popular because there was this appetite for replacing synthetic mesh with something better and something that will resist infections. A lot of research early on was promising, especially pre-clinical data, and I became a big fan of mesh made out of processed pigskin. It was supposed to be resistant to infection and not just go away again but remodeled to be similar to human tissue.
What we found through experience is that the results were very disappointing. And I personally have gone away from them entirely because as more knowledge and data came out, that became apparent. There are major drawbacks. When we looked back at our trials, we found that the rates of infections and re-operations were significantly higher in the patients getting biologic meshes. We feel like we have much more reliable synthetic meshes, and our techniques allow us to use meshes because we're hiding between layers of the abdominal wall.
What about the bioabsorbable meshes? What’s the data so far?
Dr. Novitsky: The bioabsorbable meshes do not have long-term data yet. It’s still evolving. And it's okay, but it's not as good as synthetic, so we still use it sparingly because we strive for 100 percent efficacy. You know, recurrences really hurt my feelings. We really like to minimize those! Recurrence isn’t just statistics. Every recurrence in our practice has become a sense of defeat. People say, "Even in the best hands, you're going to get some recurrences," but I can tell you in the world that we live in, it's very deflating. I don't remember the last time I truly got one, so we strive for that.
If you use the right approach and the correct mesh, and the right technique, your recurrence rate should be disappearing, and that's what we're striving for. No failures.
Let’s jump to the groin and talk inguinal hernias.
Dr. Novitsky: We do laparoscopic, open, and robotic, depending on what the patient's needs are. Robotics is a huge edge for us. I limit it to more complex scenarios because I have extensive experience in laparoscopic surgery. But robotics has become a huge addition to treating our groin patients, for people who've had previous surgeries, for more complex larger repairs, for those who need previous mesh removed, and some other scenarios for patients who are obese, so we use robotics for that.
I use laparoscopy for all straightforward (and the vast majority of) inguinal hernia patients. We use open for those who need mesh removed, for those who are a little too old or have other circumstances preventing them from getting a laparoscopic repair. We're also able to do it without mesh for those patients who desire to avoid mesh and offer reliable tension repairs as well, where we suture layers and layers of tissue in the groin under tension. So again, we have every procedure in our toolbox. During the initial consultation, we go over the risks and benefits of each approach.
It was surprising to read that in 2021, most inguinal hernias are still done with open surgery.
Dr. Novitsky: Yeah, 70 percent!
Dr. Podolsky: Oh yeah, and I would say 98-99 percent of my inguinal hernias are done minimally invasively. The majority of those are laparoscopic, robotic when needed. So the norm is completely different from what we do here.
You touched on research quite a bit, but what else is new in research? Anything you’re excited about?
Dr. Podolsky: We’re looking at several things. Like, mesh innovation practice patterns to see who's using what. We have an enormous database for our big abdominal wall reconstruction patients that we're doing a deeper dive into to see how, for instance, even the more complex patients within that cohort (the patients with liver and kidney transplants, etc.) are doing after these larger procedures. We're looking at what different medications are given during an operation and how that affects post-operative care and recovery. Most importantly, we're building a comprehensive data set of our own to track our patients, follow our patients, and really hammer down how they're doing.
Dr. Novitsky: I've traditionally been involved in a lot of hernia-related research, NIH funding and industry and societal funding, all that. Our research infrastructure at the Columbia Hernia Center is relatively young; we’re still building that infrastructure. And Dina has really led the way in a lot of this clinical research. We’re ramping up our quality improvement projects.
But in terms of the world, I always say this is such a dynamic field that it is silly to think that what we know in 2021 will be true in 2025 or 2030. It's really rapidly developing, and I'm sure there are going to be newer materials that are coming out, combinations of materials. I've counseled companies, trying to help them better understand the needs of surgeons and the design materials. So, I think that will continue to improve. The most important thing is that we remain cutting edge. There’s nothing new out there that is not in our sight. And we continue to use what we feel are the best available materials and approaches for every single patient.
On that note, what are your goals for the next five years, ten years?
Dr. Novitsky: Personally, I came here because I was interested in establishing a world-renowned center, a destination for hernia repair. I was a part of a pretty large, successful hernia center in Cleveland, Ohio prior to coming to Columbia. After I was recruited here, it was time to emphasize the need for recognition of abdominal wall surgery as a field. And that starts with training new surgeons too.
We want to continue to expand the services that we offer, to create awareness of the services that we offer locally, regionally, nationally, and continue to lead the way in optimizing hernia care—and teaching others about best practices.
Dr. Podolsky: Yeah, I would love to do a couple of things. I am excited to get some kind of stable research group, a comprehensive outcomes program for us. And grow our division into a true surgical division at Columbia. We've just really started to get a foothold here, have internal referrals, people within the system know who we are, and I really want to grow our presence here and throughout the region.
What are you most optimistic about?
Dr. Podolsky: For me, I'm most optimistic about people around the country being able to get excellent hernia work done by specialized folks who know what they're doing. And to try and change the outcomes that we've been seeing. That's really exciting stuff.
Dr. Novitsky: I can tell you my optimism stems from watching Dina learning the craft and then passing on the craft. Dina continues to lead robotic training for Columbia’s surgical program residents. Her interest and skill in robotics have made her such a leader of robotic training, and watching the fellows excel upon graduation in their jobs is the ultimate satisfaction.
It gives me a lot of optimism that we continue to exponentially spread the word and improve the overall level of hernia surgery in the United States. I'm very optimistic that this movement will only continue to grow. Complications will become much more rare, and recurrences will become rarer and rarer too. People will continue to dedicate more of their effort and time exclusively to the field of abdominal wall surgery. It's going to happen.

