New Critical Limb Ischemia program addresses all factors involved in peripheral arterial disease, providing options for diabetics and others with advanced arterial disease.
Most people are familiar with atherosclerosis, also called hardening of the arteries. Atherosclerosis is responsible for a significant number of heart attacks and strokes in the United States every year. What people may not know is that the very same disease process — buildup of plaque within the heart blood vessels — can affect the arteries in the rest of the body as well.
When it occurs beyond the heart, blockage of the arteries is called peripheral arterial disease, or PAD. Patients with coronary artery disease are at risk for PAD and vice versa; the risk factors for both diseases include obesity, diabetes, hypertension, high cholesterol, cigarette smoking, and family history.
 PAD most commonly affects the legs, but may occur elsewhere as well, says Danielle Bajakian, MD, Assistant Professor of Clinical Surgery, Columbia University College of Physicians and Surgeons, and Director, Critical Limb Ischemia Program, NewYork-Presbyterian Hospital/Columbia University Medical Center. Even if a person has no symptoms, the presence of PAD still indicates systemic disease that must be addressed. When symptoms do appear, they usually begin with claudication, or cramping in the back of the leg while walking. Such pain usually stops during rest, and then resumes while walking. Symptoms may occur in just one leg. "Mild disease can usually be treated with changes in lifestyle such as losing weight, smoking cessation, exercise, and managing blood glucose and cholesterol levels," says Dr. Bajakian.
PAD most commonly affects the legs, but may occur elsewhere as well, says Danielle Bajakian, MD, Assistant Professor of Clinical Surgery, Columbia University College of Physicians and Surgeons, and Director, Critical Limb Ischemia Program, NewYork-Presbyterian Hospital/Columbia University Medical Center. Even if a person has no symptoms, the presence of PAD still indicates systemic disease that must be addressed. When symptoms do appear, they usually begin with claudication, or cramping in the back of the leg while walking. Such pain usually stops during rest, and then resumes while walking. Symptoms may occur in just one leg. "Mild disease can usually be treated with changes in lifestyle such as losing weight, smoking cessation, exercise, and managing blood glucose and cholesterol levels," says Dr. Bajakian.
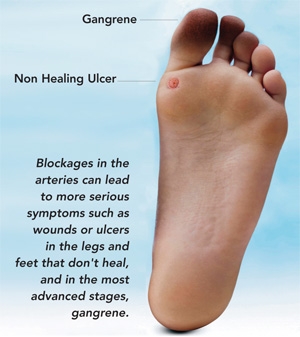
If PAD progresses, blockages in the arteries can lead to more serious symptoms such as pain in the feet while lying down, wounds or ulcers in the legs and feet that don't heal, and in the most advanced stages, gangrene. This occurs more commonly in patients with diabetes or who smoke cigarettes but can occur in anyone. These symptoms indicate critical limb ischemia resulting from impaired circulation, and if untreated, could result in amputation of the leg. Moderate or severe disease may require treatment to open the blood vessels to restore circulation. "People with diabetes face a particular risk for critical limb ischemia," cautions Dr. Bajakian. "Up to 20% of diabetics may eventually lose a limb if preventive measures and careful medical and surgical management are not part of their care."
 To address the unique needs of diabetics and other patients who have PAD (or are at risk for it), the Division of Vascular Surgery and Endovascular Interventions at NewYork-Presbyterian/Columbia has established a dedicated program for the prevention and treatment of critical limb ischemia. This multi-disciplinary, comprehensive program not only treats PAD, but works with patients to treat all underlying risk factors. Formalized in 2010, the critical limb ischemia program includes a collaborative team of experts: vascular surgeons, endocrinologists, cardiologists, podiatrists, wound care specialists, and imaging specialists. The program offers many treatment options that are unavailable elsewhere, including the latest endovascular techniques for restoring circulation to both large and small arteries in the legs. "In most places today, patients see multiple doctors who each address a single problem, but do not communicate with one another. Results for patients are not optimal," explains Dr. Bajakian. "Many patients need care for multiple problems, and receiving coordinated care is far more effective." She stresses that anyone who experiences pain in the legs with walking, or wounds that don't heal in six weeks — and particularly anyone who is overweight, has diabetes, or smokes — should seek an evaluation by a critical limb ischemia specialist "expeditiously." As Dr. Bajakian explains, "If you wait, it may be too late. The sooner you go in for evaluation, the higher the chance your leg, foot, or toes can be saved." She also notes that while many patients have been told elsewhere that they could not be helped, the program at NewYork-Presbyterian/Columbia can often provide treatment options. "Because of our comprehensive expertise, many times we can offer further treatments and save a limb when others cannot."
To address the unique needs of diabetics and other patients who have PAD (or are at risk for it), the Division of Vascular Surgery and Endovascular Interventions at NewYork-Presbyterian/Columbia has established a dedicated program for the prevention and treatment of critical limb ischemia. This multi-disciplinary, comprehensive program not only treats PAD, but works with patients to treat all underlying risk factors. Formalized in 2010, the critical limb ischemia program includes a collaborative team of experts: vascular surgeons, endocrinologists, cardiologists, podiatrists, wound care specialists, and imaging specialists. The program offers many treatment options that are unavailable elsewhere, including the latest endovascular techniques for restoring circulation to both large and small arteries in the legs. "In most places today, patients see multiple doctors who each address a single problem, but do not communicate with one another. Results for patients are not optimal," explains Dr. Bajakian. "Many patients need care for multiple problems, and receiving coordinated care is far more effective." She stresses that anyone who experiences pain in the legs with walking, or wounds that don't heal in six weeks — and particularly anyone who is overweight, has diabetes, or smokes — should seek an evaluation by a critical limb ischemia specialist "expeditiously." As Dr. Bajakian explains, "If you wait, it may be too late. The sooner you go in for evaluation, the higher the chance your leg, foot, or toes can be saved." She also notes that while many patients have been told elsewhere that they could not be helped, the program at NewYork-Presbyterian/Columbia can often provide treatment options. "Because of our comprehensive expertise, many times we can offer further treatments and save a limb when others cannot."
ENDOVASCULAR PROCEDURES FOR PAD
The Critical Limb Ischemia Program offers every available therapy to restore blood flow to the lower extremities, including new therapies to treat smaller vessels. Over 90% of patients who require surgery can be treated with minimally invasive endovascular techniques rather than open surgery. These minimally invasive techniques are performed under sedation and local anesthesia rather than general anesthesia, and most patients return home the following day.
- Angioplasty: After accessing the blockage through a catheter, angioplasty involves placing a balloon in the affected area and inflating it to keep the artery open.
- Atherectomy: Using mechanical devices (inserted through a catheter) to remove plaque in the artery.
- Stenting: Placement of a wire mesh strut within a narrowed area of the artery in order to keep it open.
The critical limb ischemia program is actively researching new technologies including stents, bypass grafts, gene therapy, and autologous stem cell therapy to promote growth of new blood vessels. Learn more at www.columbiavascular.org
