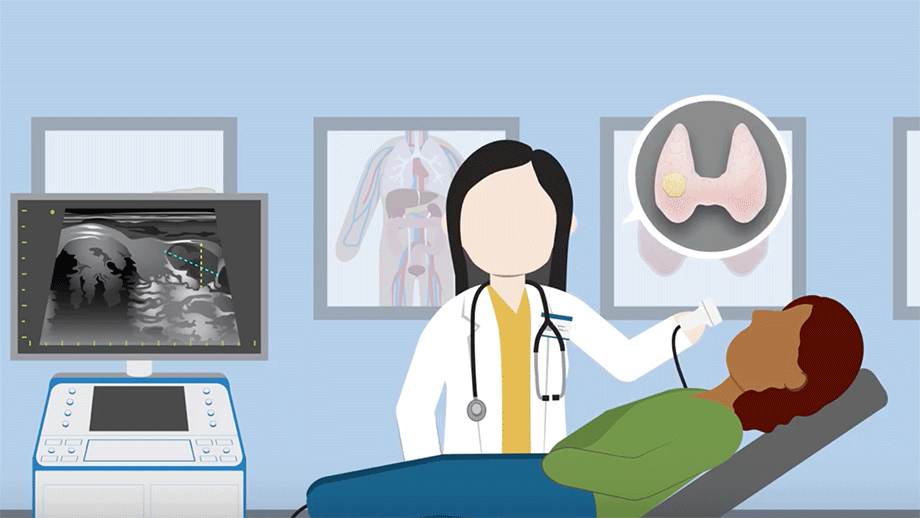
Radiofrequency Ablation (RFA) is a non-surgical technique that can safely and effectively treat non-cancerous thyroid nodules. Many people, however, don’t know it is an option. They mistakenly believe that their only recourse to treating a nodule is surgery.
Nicole is a recent recipient of RFA. She had the procedure a year ago, here at Columbia, under the care of Dr. Jennifer Kuo.
Nicole has generously shared her experiences, below. The hope is that those in a similar situation can learn what options are available to them and what to expect if they choose RFA as their treatment.
JUMP TO A SECTION:
- SYMPTOMS & GETTING DIAGNOSED
- EXPLORING TREATMENT OPTIONS
- FINDING AN RFA PROVIDER
- COSTS & INSURANCE COVERAGE
- RFA: THE PROCEDURE ITSELF
- POST-PROCEDURE
- FOLLOW-UP ULTRASOUNDS
- REDUCTION IN NODULE SIZE
- TAKEAWAYS
SYMPTOMS & GETTING DIAGNOSED
I first got diagnosed with a thyroid nodule that was found by my primary care physician, sometime in 2015 or 2016. He felt it in my neck during a routine exam.
I don’t recall the exact reason for the visit. It’s possible I was there because I had a cold, and he was feeling my lymph nodes with his fingers. And just feeling around my neck he was able to tell that there was a little lump there. He said, "Oh, what's this? You should maybe have that checked out."
He had me go in for an ultrasound, which confirmed it. The doctor wanted the nodule tested for any cancer cells initially. So I had a biopsy. This was a fine needle aspiration (FNA), which is where they go in and they take a sample from the nodule and test it for cancer. It was benign.
Knowing it wasn’t cancerous, we determined to monitor it through ultrasounds. I had it continually monitored, maybe annually, or every other year, to check it for growth. And it did steadily grow over a few years.
Eventually it got to a point where it was just getting large. Now, my situation was a little more unique than maybe others might experience, in that I had a large thyroid nodule, but it didn't present very large.
When looking at me, the right side of my neck might have looked a little bit larger than the other side, but it really wasn't a large bulge and it didn't show that much. I also didn't have symptoms.
Some people might experience difficulty talking or swallowing or breathing, and I didn't have any symptoms. It was just this large benign nodule that kept growing.
Every couple years, it got a little bigger. So I was never at a point where I wanted to have a surgical procedure done because it was a surgery for something that wasn’t bothering me. It was, at that point, just cosmetic.
But it did keep growing, and I was starting to get nervous, because at some point, the larger that it got, it might be more difficult to have it removed.
EXPLORING TREATMENT OPTIONS
I had talked to doctors (primary care, and ENTs) about having it removed in the past. That would involve removing half the thyroid gland. That's pretty much the only option that's widely available. That was certainly the only option available where I live.
If I had to go to a surgeon to have the surgery done, chances are half of my thyroid was going to start either over-producing or somehow overcompensating when it came to thyroid hormone. Maybe, maybe not. There was a chance that I might have to be on thyroid hormones for the rest of my life, if not. There are also other inherent risks that can come along with surgery.
FINDING AN RFA PROVIDER
So that's when I started looking into the radiofrequency ablation. Of course, I just went online and I was looking at thyroid nodules and researching different treatments that are available, other than surgery. And RFA came up in my search. It was hard to find!
The problem is there really aren't a lot of facilities that are offering this procedure. I was really surprised that it's not being offered at various esteemed facilities where they have so much state-of-the-art equipment, many doctors and so countless treatments that they do for their patients. Yet, a procedure like this isn't offered there.
I had to try to start finding places to even meet with a doctor to see if this would be a viable option for me. Because you don't really know, until they look at your history and condition and determine if it's going to be a good fit for your condition and needs.
I ended up doing research online and trying to just find places around me that even offered it.
So I had found that Mount Sinai was one hospital, and when I called them, they said, "Nope, we're not doing it anymore." And then there was a doctor in Boston that was offering it, and also one somewhere else in Pennsylvania, maybe. But the Pennsylvania doctor would not see me, remotely. They would not do any telehealth with a patient in New York. So that one was out.
The doctor in Massachusetts was able to do telehealth. And I actually did end up doing a consultation with that doctor over the phone.
Columbia was the other option. So I called. They were immediately very helpful.
Dr. Kuo was willing to do the remote appointments through Telehealth with me, at least to start, for a consultation. She was also able to remotely review all of my records. I had everything sent over there.
I ended up going with Columbia because the other doctor in Massachusetts was not as experienced as Dr. Kuo. He hadn't done as many procedures, and Dr. Kuo was very experienced. She was able to talk to me about different patients that she's treated and about different scenarios and situations.
So I ended up going there, and I do live in New York, so it was just a lot easier for me to have everything done with insurance and being in the same state, it just made more sense.
COSTS & INSURANCE COVERAGE
What was very helpful is that Columbia was able to give me the cost of the procedure upfront. I want to say it was $3,500, at the time. There was also a $150 ultrasound fee. I don't know if these costs have changed, since when I had the procedure done in November 2021. But that's what the charges were.
They were able to give it to me up front. They said, "We don't know if insurance is going to cover this or not. So this is what it's going to cost you to have it done." Now, I could plan. At least I knew that if I didn’t have insurance coverage, I would need to have this money allocated to have the procedure done. I was able to plan for that. And then, it would be a happy surprise if insurance covers it.
Well, my insurance did end up covering it, and I wasn't planning on them covering it. I learned that, in most situations, insurance did not cover this procedure for various reasons. My insurance ended up covering it, and I want to say I ended up paying a couple hundred dollars. (I am a federal employee, so I was insured through a government plan, which was at the time participating in the Aetna network. I would hate to offer false hopes of coverage, however, so I cannot state whether or not this continues, today).
RFA: THE PROCEDURE ITSELF
I don't think that there was much involved in prep for the procedure when I went in. In fact, I think I walked into the room and maybe they took my blood pressure and said, "Okay, let's get started." I really don't think there was much that we went over from what I recall.
The way that the procedure is done is that they numb the area, first. It's just a local anesthetic, so they will numb the area with a needle. Then I think there's a needle probe that is inserted into the nodule. The probe is connected to a machine that makes weird noises. The needle then heats up inside.
The best way I could explain the sensation is that it felt like an intense yet tolerable burning inside of my neck, as the machine would ramp up. Perhaps more than I’d anticipated, but tolerable, still.
There are different settings on the machine. Dr. Kuo would dial it up and then it would just increase, and this intense burning sensation would begin. It would also make weird popping noises, which was very strange as well. So it was a weird sensation. And a bit uncomfortable.
Fortunately, I could communicate with Dr. Kuo throughout the procedure. I could say, "Okay, it feels like it's burning, it's hurting a lot." I could communicate how it was feeling with the doctors.
When the burning felt too intense, Dr. Kuo would say, "Okay, let's give Nicole a break, turn it down a little bit." And then it wouldn't be as bad. And the procedure is not constant, but start-and-stop, wherein the pain alleviates between “zaps.”
The other notable sensation during the procedure was a feeling of pressure. They had me suck on ice chips to alleviate that and pressurize.
As a comparison to getting a tattoo, the burning from RFA is more intense. But, unlike a tattoo, it starts and stops. A tattoo is more of a constant pain, whereas RFA would ebb and flow.
An important thing worth mentioning is that I had a larger nodule. It measured a little over five centimeters. So it's considered a pretty large size as far as a thyroid nodule goes. And mine was “vascularized,” so it had a lot of blood flow.
Therefore, Dr. Kuo explained, she had to focus on certain areas and really ablate a lot in those areas to kill the blood flow.
Since pain is subjective, and different nodules will have different characteristics, suffice it to say it was intense but tolerable.
I think the procedure, in all, was maybe an hour, start to finish. (I think Dr. Kuo said that she had to do the actual ablation for 45 minutes). And so that might vary from person to person, depending on the size of the nodule and whether the nodule vascularized. So it's maybe different for every person. But I did find the whole thing to be tolerable.
POST-PROCEDURE
Afterwards, I did end up a little swollen and uncomfortable in my throat. My mom took me to the appointment and then drove us back to the hotel (we stayed in a hotel across the bridge in New Jersey). Then the next day, we drove home.
In terms of aftercare, they just had me use ice packs on my neck. Maybe a higher dose of Motrin, but I didn't really take much in the way of painkillers. And it was sore and it was tender, but it was not horrible. It was tolerable.
In fact, I did some of the driving on the way home even the next day. My neck was just a little sore. I didn't have full range of motion, but I was able to drive.
I was able to go back to normal business, but just somewhat restricted. I think I might have taken a day off of work and just iced my neck, kept it somewhat still and kept my head elevated.
As for my job, I work at a computer, so I was quickly able to go back to work and do normal things. About a week or two after the procedure, the swelling went down. Everything seemed back to normal.
FOLLOW-UP ULTRASOUNDS
Dr. Kuo prescribes an ultrasound to check the status at one month, three months, six months and twelve months. Dr. Kuo's so helpful in being able to treat me away from New York City and doing things remotely.
So I go to the ultrasound tech where I live. I get the images, and then I'm able to upload the images to Columbia's portal, on which I can share the images and results. Dr. Kuo’s incredible team walked me through each step. I just get the disc and upload it for them. This way, Dr. Kuo can look at the images. The ultrasound technicians also send over their report, and then Dr. Kuo gives me a call and we talk about it.
One surprising event occurred, right around the first ultrasound. All of a sudden, my neck swelled up. It was getting sore and didn't feel very good. I was getting really nervous that something was wrong. But I got the ultrasound done, they said nothing looked out of the ordinary.
Dr. Kuo looked at the ultrasound and everything looked fine. She pretty much put my mind at ease and said, "That can be normal, just to have some swelling and things even a couple months, or a couple weeks after the procedure." So she was right. About two weeks later, it was fine again. I haven't had any issues since.
REDUCTION IN NODULE SIZE
I've been having the ultrasounds done, and the nodule has continued to show a decrease in size, each time.
The nodule started at around 53 millimeters, and then at one month ultrasound, it went down to 44 millimeters. So it decreased 10 millimeters in size.
Three months out, it measured 31 millimeters: another 10 millimeters down. At six months, it was 29 millimeters. And currently, at 12 months, it hasn't really changed.
So, it's gone from 53 down to 29 millimeters in size. And now, you can't even see it.
There is no marking on my neck. There's no evidence of any procedure or anything. So it didn’t leave a scar.
I still have a small nodule in there, but you can't see it. It has never bothered me, so it doesn't matter to me. And Dr. Kuo pretty much left it at, "Okay, well, there is nothing more we need to do. We'll just monitor it. Every year, we'll have you do another ultrasound. And as long as you're comfortable with it, at the size it is now, no further treatment is needed." And I was happy with that.
TAKEAWAYS
I told Dr. Kuo after our call the other day, this was the right decision for me. I was so happy that I didn't choose to undergo surgery and anesthesia and having to have my thyroid removed. But I knew that the larger the nodule grew without intervention, the harder it would be to remove, the bigger a scar might remain from its removal, and the more likely I might be to develop symptoms.
In the end, RFA really was a good decision and I'm glad that they offer it.
I found there really isn't that much information online. There are some studies and I think Columbia's website has the most information about it. I think there's maybe an article about Dr. Kuo and the procedure that I thought was probably most helpful. But because it's not offered that widespread, it's hard to find a lot of information.
When I first started researching, I didn't even know if this was something that would work for me, with the size of my nodule, or if it was even a procedure that would be recommended. I didn't really have any place to go or anybody to ask.
So, if I was to give advice for someone who is in a similar situation that does not want to have to go the route of surgery, I would definitely consider it as an option and call Columbia and see if they can set up a consultation with Dr. Kuo.
The only downside is that, if you don't live locally, you have to travel. There could also be reasons that you may have to travel again, if you're not seeing the results that were anticipated. It is also a possibility that you may have to go back for a second procedure in the future if it were to regrow, which is maybe not likely, but could happen.
You have to weigh all the risks, like with anything. But in my opinion, I think that the benefits outweigh the risk of surgery.
FURTHER READING:
- Thyroid Center Home
- Thyroid Nodules
- Thyroid Biopsy Clinic
- Interventional Endocrinology
- RFA: What to Expect